The simple solution to prevent fractures
I am currently eyeballs deep in research on bone health and fracture prevention.

As ever when you think you know something, when you read deeper, things are never quite as clean cut as you thought and the general narrative on the subject isn’t really representative of the research.
Frankly, once you start really deep-diving into a subject, you realise we are drowning in research, that is :
a) Extremely poorly written
b) Extremely poorly designed, either by people wanting a specific outcome or by people who simply do not understand the subject they are studying.
c) Many of the benefits/associations may be statistically “significant” but they are so small they are clinically meaningless.
The end result is the amount of research is overwhelming and it is challenging to hear signal amidst so much noise.
It is abundantly clear in the world of bone health that a diagnosis of osteoporosis via bone mineral density scan is King (or Queen).
But really, what we want is fracture prevention, because every year, many people fracture and have normal bone density.
Equally, there are lots of elderly people with osteoporosis that never fracture.
Now there is a rabbit hole you can go down on bone quality vs density but this is not the place for that, CCCN members will get that shortly.
The reality is that BMD can predict future fracture, though the predictive value of BMD scans are far higher in people of 50 years of age than those of 70 and upwards (because a low BMD in a 50 year old is very abnormal while a low BMD in an 80 year old is not, so you lose the predictive value).
Moreover, the other issue with BMD to predict is it also misses lots of people who still go on to fracture.
That is because density does not equal strength per se.
In fact 50% of fractures in the community occur without any osteoporosis present.
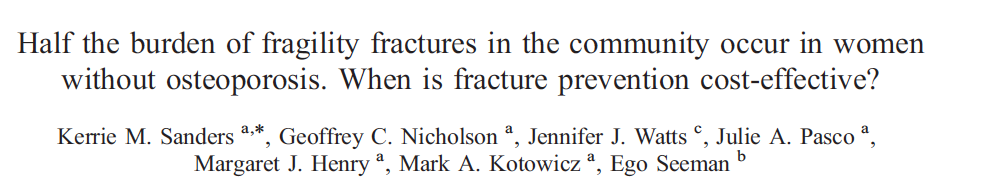
Think about that.
How many patients who do not have osteoporosis on a DXA scan but do go on to fracture could be saved with diet, exercises, supplements?
Think also how many people with a low BMD who would never have fractured are treated unnecessarily.
We also need to remember that it is hip fractures that are usually more devastating to older patients’ health.
It is this last point that we should consider in terms of fracture reduction.
In my mind, it is overwhelmingly the elderly who are falling that are going to fracture.
So, if we can stop or reduce the falls, then we can stop or reduce the hip fractures.
In the course, we like to keep it simple but effective. Try this for size:
If you are elderly and cannot balance on one leg for more than 10 seconds, then your risk of all fractures, but especially hip fractures, goes up dramatically.
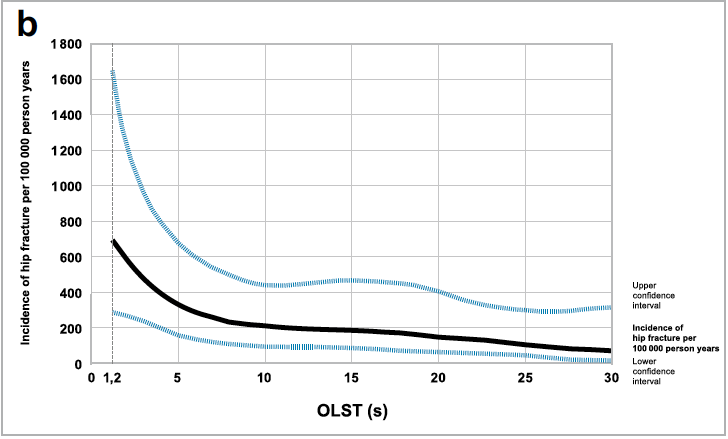
The risk is independent of bone mineral density, but when combined with it, the predictive risk factor was even higher.
This is so simple and the benefits of simple balance training are massive.
Remember also to get them to eat protein with every meal.
Muscles are made from amino acids.
No protein = muscle loss, or sarcopenia.
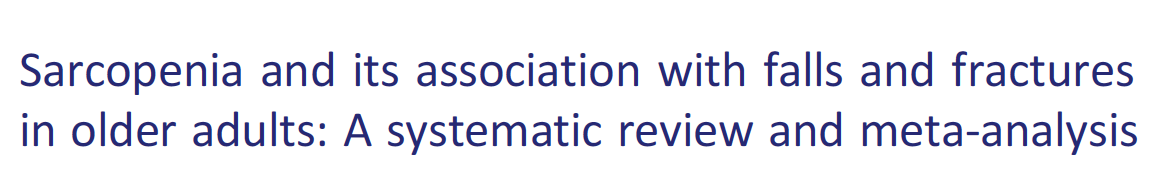
And sarcopenia = falls and fractures.
That means eating meat/fish, eggs, nuts, beans, lentils, possibly a protein powder or even better essential amino acids that need no digestive effort at all.
As we age, our stomach acid levels will slowly drop and this means breaking down protein gets harder and food, especially protein, can sit in the stomach.
For this reason, older patients often end up eating less protein and more carbs but often less food in general, they lose their appetite.
Many of the very aged are woefully deficient in many key macro and micronutrients.
This is where a high-quality multivitamin plus added magnesium and vitamin D in therapeutic doses is ideal.
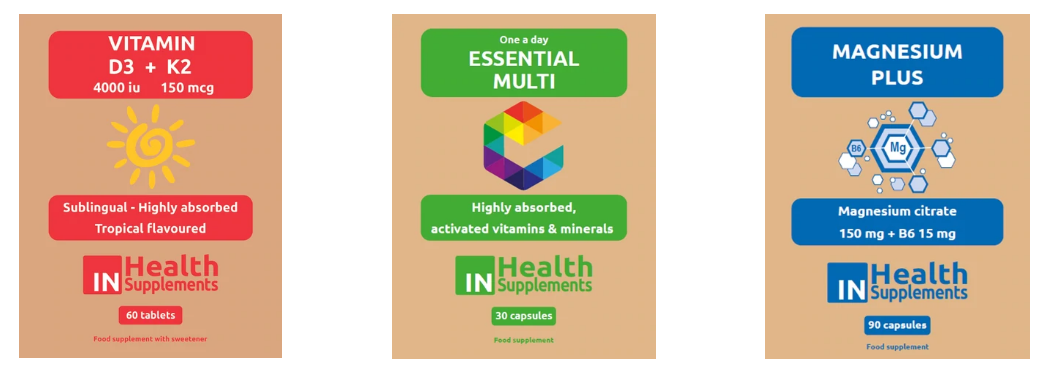
They have a gap between what they need in terms of nutrition and what they are eating and absorbing.
Those gaps must be filled with supplements.
We even have a lesson on the CCCN course dedicated to it.
I always say to patients this is just a trial for one month to see how you feel – energy, mood, aches and pains.
I cannot remember the last time I gave out these three and patients did not report an improvement.
ACTIONS TO TAKE:
– Try some apple cider vinegar “with the mother” for older patients that are struggling to digest protein. The extra acid might really help them.
– Get the Core 4 IN Health Supplements in clinic and see the changes optimal nutrition makes to your patients’ results from care.
– Start testing balance. We want 10 seconds or more, get them balancing with feet together, then feet one in front of the other, then on one leg.
