Did you see the recent news on Vitamin D?
Did you see the news?
A few weeks ago we talked about evidence based nonsense and why the drive for RCT’s to “prove” everything has left us in a place David Sackett, the “founder” of EBM, did not anticipate or like.
The reality of RCT’s is that they are designed to change one thing, to “prove” the one thing causes condition X or one drug/intervention has a “significant” effect of condition X.
The challenge is this all assumes that there is only one thing that is the issue, or the patient only needs one thing to be treated.
In a research setting this works if you are suppressing a symptom or system, because we know you can achieve that very well with pharmaceuticals.
The challenge is when you are looking at nutritional interventions, you cannot suppress a symptom or system in quite the same way (and you really should avoid playing medicine with supplements if at all possible).
What we are looking at is can we allow the body to work more optimally to allow normal function of the systems and healing.
At the centre of the Core Concepts in Chiropractic Nutrition is the basic idea that we need a certain amount of “good” stuff and a minimal amount of “bad” stuff.

After all we are simply a series of pathways with building blocks at the start and vitamins and minerals as co-factors for enzymes modifying these into final products, be it a hormone, a neuro-transmitter, new collagen or energy.
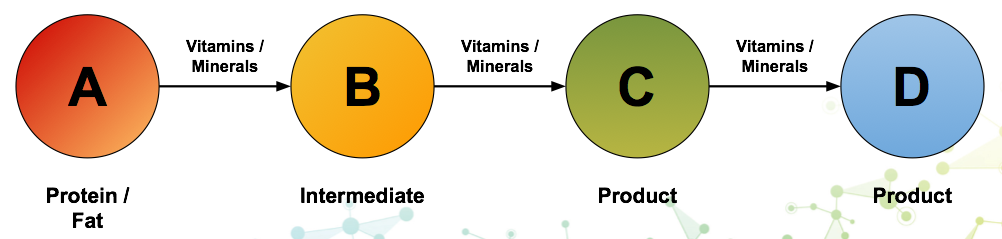
Not enough good stuff to building or facilitate the pathway means less end product.
Too much bad stuff like infections, toxins, bad foods, slow the pathways down, and thus less end product.
In this scenario, we need to use “common sense medicine”.
Whilst you do get the occasional silver bullet to create massive shifts in someone metabolic system, we have to recognise that human beings are complex systems and often there are multiple things in play, often affecting each other.
So only changing one thing, often yields disappointing results.
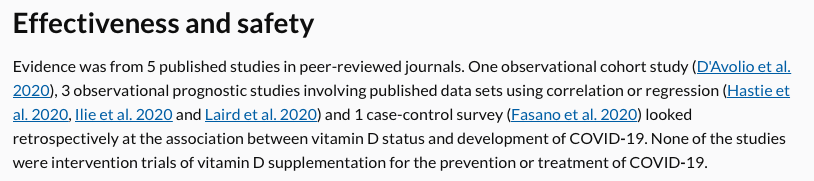
In the case of vitamin D and COVID-19, the NICE reviewers rather had their hands tied by the idea of one thing to stop the virus.
They have correctly pointed out that there are only 5 specific COVID vitamin D specific studies, none were RCT’s, none were interventional, did not adjust for other variables etc.
Now to be fair from a “scientific research” POV this is all correct and as NICE reviewers they had no choice.
https://www.nice.org.uk/

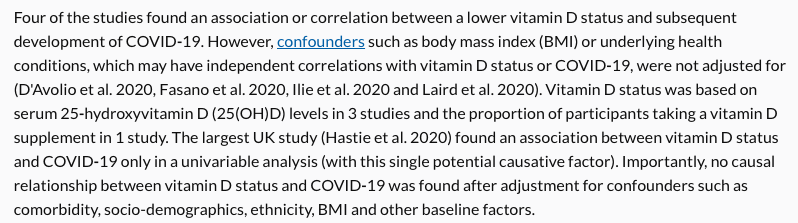
But is the idea that vitamin D on its own is the one thing that is causing higher deaths in BAME groups likely?
How about we use some common sense and ask the question: Is vitamin D an important part of a healthy normal functioning immune system?
If yes, then we ask: Are people with darker skin tone more like to be deficient in the UK?
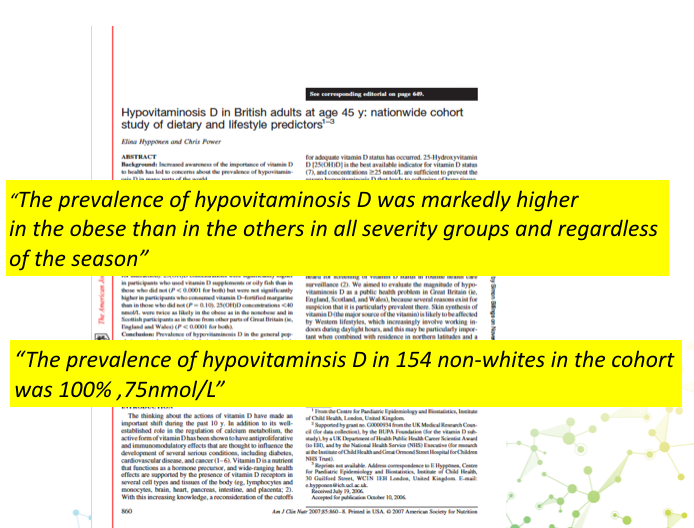
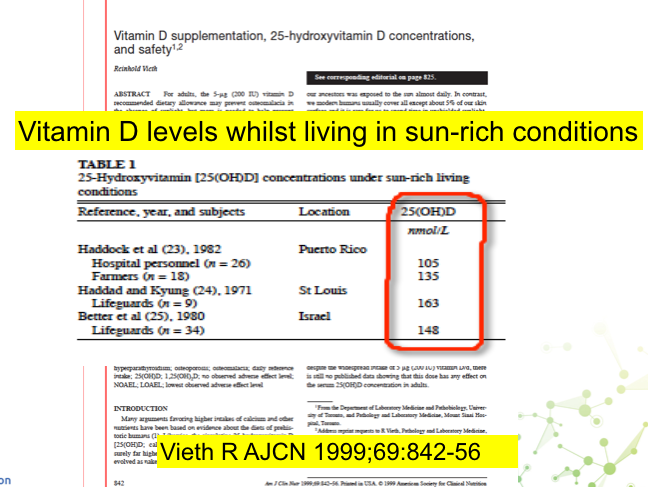
If, yes what blood level of vitamin D might they achieve if they were living in a latitude suited to their ethnicity.
The goal should then be to ensure, the members of the BAME groups have a blood level above 100 nmol/L as part of an overall health strategy to enhance and optimise their immune system to help prevent death from COVID-19.
The review does suggest that people with darker skin tones should “consider” taking 10 mcg/400iu of vitamin D all year round.
Given the research on deficiency in BAME groups I take exception the word “consider”, it should be “must”.
The dose is also simply inadequate.
Their goal is for BAME groups to be not deficient ie above 50 nmol/L.
This again I take exception to given the blood levels achieved by people living and working in sunny climates of suitable latitude to their ethnicity.
But even if that was an acceptable goal, 10mcg/400iu will raise the blood level of an average size person around 10 nmol/L.
Rule of thumb is per 25mcg/1000iu raises blood levels by 25 nmol/L.
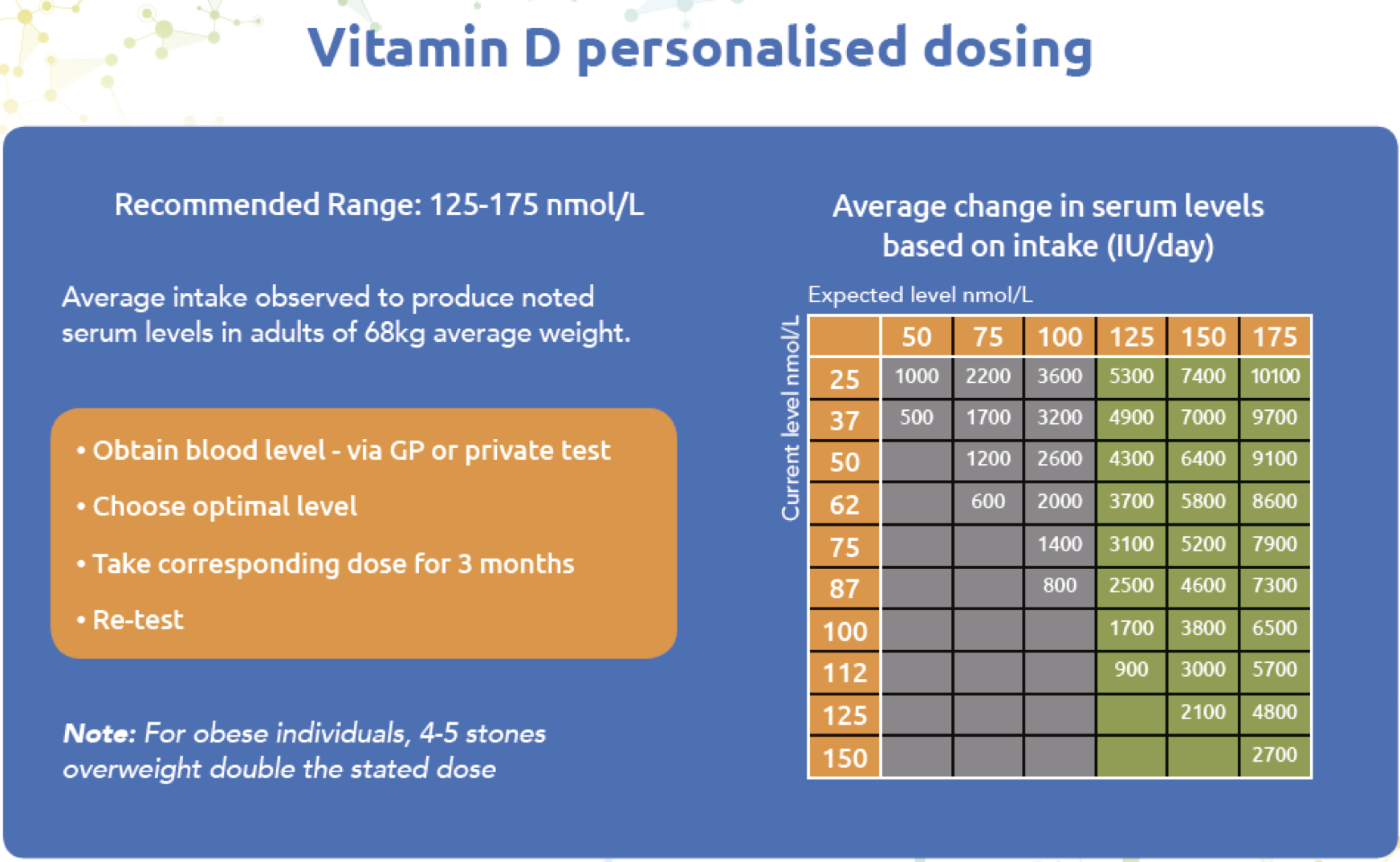
So let us suppose your ethnic ancestry is from central Africa and so you have very high melanin skin content and have levels of 15 nmol/L.
A daily dose of 10 mcg/400iu will (on average) get you to 25 nmol/L, still woefully deficient.
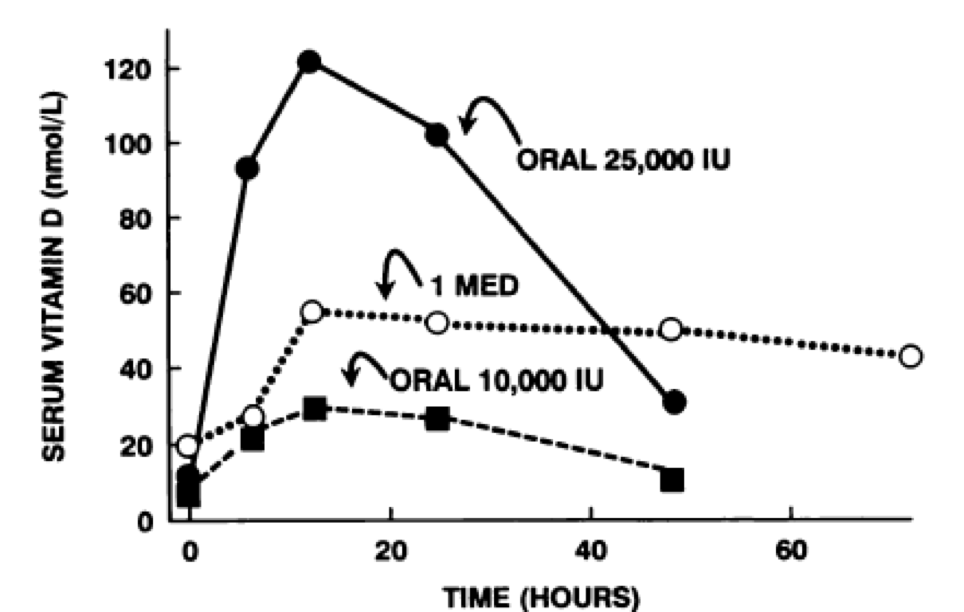
A daily dose of around 125 mcg/5000iu would safely achieve levels above 100 nmol/L – remember sun exposure can achieve up to 20,000 iu of vitamin D in 30 minutes.
Check the graph below, 1 MED = slightly pink skin, gave higher levels of vitamin D than an oral dose of 250mcg/10,000iu
But if they are obese it gets even worse, they often need double the dose to achieve normal levels.
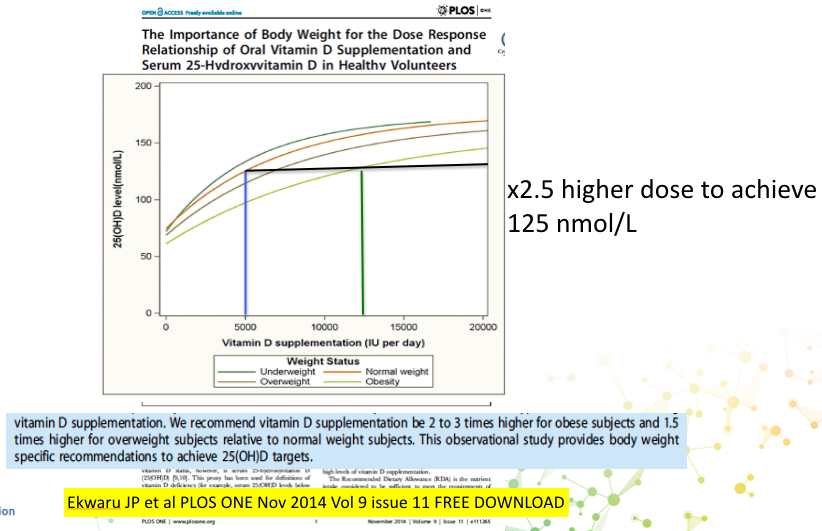
Vitamin D is a fat and so is stored in the fatty tissues, thus reducing the available vitamin D for circulation into the cells.
Understanding the biology of vitamin D allows us to apply common sense to our advice
ACTION TO TAKE
– Use the patient education videos on my personal website to educate your patients on vitamin D production, symptoms and dosing. These are part of the evolving “IN Health System” a patient education library so you don’t have to keep saying the same stuff again and again and again.
https://integrativecare.co.uk/
– If in doubt about levels, test, it is only £29 finger prick test.
