Why sugar makes you stiff
Last week we went further into blood chemistry analysis, and this week, we are talking sugar.
Just a few days ago, I was tucking into gluten and dairy-free salted caramel cake, celebrating my 44th birthday.
It was just heavenly.

It is mainly cashews, coconut and chocolate, which are all plants, so it is pretty much as good as eating salad in my book.
So it is good that I am currently sporting a Libre 2 freestyle continuous blood sugar monitor.

It is fair to say at times I can be a slave to my hypoglycemic drops, so thought I would get some real-time data on those.
This will be especially interesting in long days at the clinic, where it is fair to say things can get a little stressful with a full clinic load.
I am still playing with the data and need to make sure I add in all the food I am eating to see what effects it has on my levels and see if that correlates with any loss of good cognitive function or just being an angry t**t (my wife’s words not mine).
Check out yesterday’s levels, which given it was my daughter’s 11th birthday party, were pretty good !

Happy birthday Iris, what a fantastic human being you truly are.

Anyhoo, back to sugar, the one area where after many years of living in a black and white, you are either healthy or suddenly diseased world, the NHS a few years back finally twigged that people do not develop diabetes overnight.
It turns out there is a spectrum! Who knew!
So the long term assessment for blood sugar control, HbA1c, was given a normal level, pre-diabetic and diabetic.
Hb is haemoglobin, the rest of it well doesn’t really matter. Ultimately it is also known as glycosylated haemoglobin.
Glycosylation is the binding of a carbohydrate (glucose in this case) to protein (haemoglobin in this case) or fat.
Keep it simple, sugar makes stuff sticky.
Get something sugary on your fingers, and they become sticky. In this case, it is the sugar binding with the protein in your skin.
Why haemoglobin for blood sugar?
Because it is long-lived at 120 days per RBC, we get a long-term assessment of how well your blood glucose levels are stabilised.
The more above normal your glucose you have, the stickier the haemoglobin you have, thus the higher your HbA1c will be.
Now the issue here is once glycosylated, it can then become an advanced glycosylation end product, or for short, an AGE.
These are permanent, and the real issue with AGE’s is they bind to protein/fat and change their function.
This is the fundamental basis for diabetic damage, be it nerve or artery.
AGE’s binding to protein and stopping it from functioning normally.
So that capillary no longer works so well, and you lose circulation.
Or binds to a peripheral nerve, and you lose sensation.
Have you noticed how badly diabetics heal?
And indeed respond to care, so stiff!
This is partly due to glucose binding to your collagen, creating an AGE and suddenly, your collagen/fascia no longer stretches like it used to.
Collagen is exceptionally long-lived, so the effects are cumulative.
AGE’s trigger more deposition of collagen, and you get crosslinking as you do with scarring from trauma.
Thus, they get stiffer and the tissue is more likely to fail and respond to care poorly.
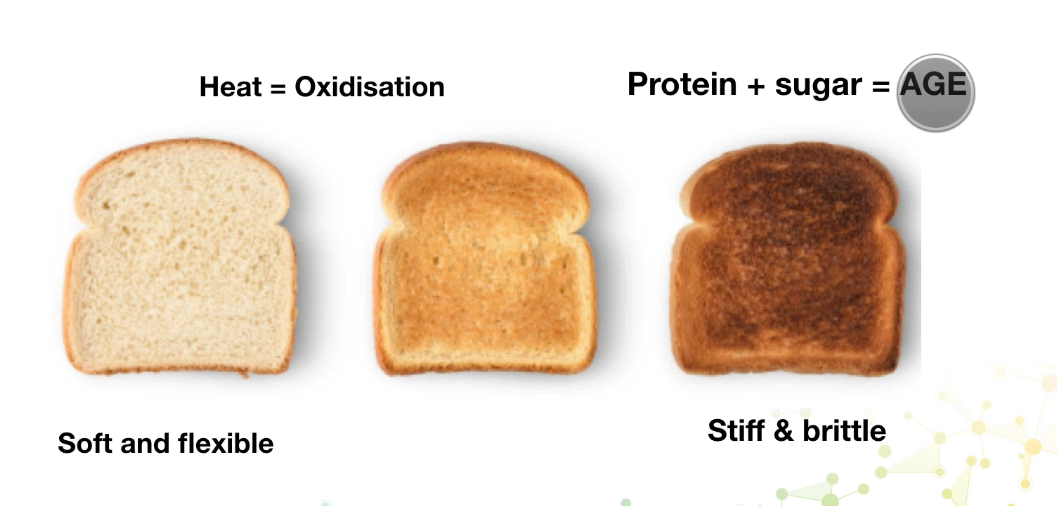
It is the difference between soft pliable bread and stiff breakable burnt toast.
ACTIONS TO TAKE:
– HbA1c: Keep it under 48 mmol/L at the very least, ideally under 42 mmol/L.
– Even if your patients do not have diabetes, make a point of telling them sugar makes you stiff. Give them the example of the sticky fingers with coke or sweets and tell them that is happening inside you. This could be part of why you hurt, why you are not responding as planned.
– If you have diabetic patients, send them to www.lowcarbprogram.com
