Why “normal” blood test levels are not good enough
One of things I frequently hear from patients is “the GP ran some bloods tests and said they are all normal”.
Now the issue here is, we have no idea what they tested for and what the actual levels were.
NHS blood tests can give a wealth of information if you know what you are looking for and how to interpret them. 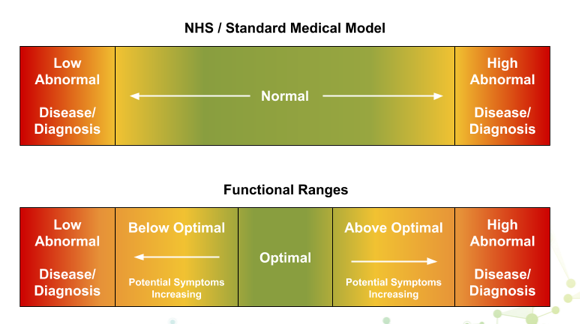 That is why I always get patients to request their blood tests from the last few years. These days they often have access online to their own results, if not, they can request them on the phone to be printed and collect them.
That is why I always get patients to request their blood tests from the last few years. These days they often have access online to their own results, if not, they can request them on the phone to be printed and collect them.
I would strongly recommend you do not get involved in requesting notes. It requires their written consent and GP’s have very little interest in passing them onto 3rd parties. It used to involve a huge amount of repetitive requests from our reception to the GP’s, and was frankly a pain in the a**e.
So today is the first in a series of cheeky tit-bits of golden nuggets or clinical pearls, whichever you prefer for interpreting blood tests from a functional POV.
Alkaline phosphatase – this is not the most common marker you will see, but it is very useful in a way the NHS doesn’t quite realise.
It is an enzyme (alkaline phosphatASE – the ase makes it an enzyme, which makes it a protein which accelerates a chemical reaction), found mainly in the liver and bone.
It has a maximal activity at pH of 9-10, hence ALKALINE phosphatase.
It is also a member of the metaloenzymes family, and these enzymes need a metal as a cofactor to be active and that metal is ZINC (this is really important).
If levels are higher than normal, usually over 130 iu/L, then either we have an obstruction somewhere in the biliary tree or some kind of liver damage.
The GP’s should take an interest in this, though this does vary quite a bit depending on the other liver related markers and the patients patient’s symptoms.
You can also get an elevation with metastatic bone cancer as the body tries to repair the damage, the enzyme activity goes up.
The NHS standard is to only take an interest in high levels and these do often indicate a significant issue. But remember we said the enzyme was ZINC dependent?
So, if the activity of the enzyme is under 70 iu/L, then one possible cause is zinc deficiency/insufficiency.
Here is a recent test from a patient:

NHS low only kicks in at 30 iu/L and to be fair they have little interest in that.
Low zinc may give symptoms around taste perception and we know there is a virus knocking around at the moment that might have an impact on that and zinc is very important to the immune system.
There are a few theories around that, nothing for sure, but interesting.
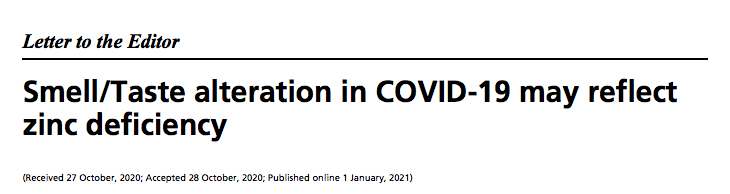
And we also know that low patients with low zinc on admission from C19 do worse than those with normal levels, much worse.

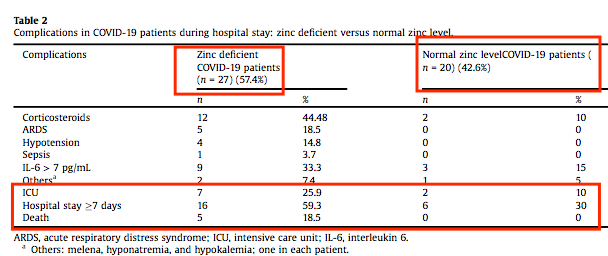
Remember that zinc is also great at stopping viral replication too.
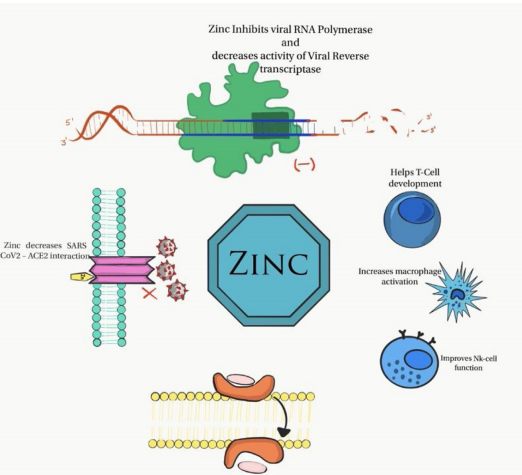
That is why we always want to keep the zinc acetate lozenges in the cupboard and use them every 2 hours for 2-3 days to ward off infections.
We talked about it here:
https://lessons.
Remember to also have a look at their nails, multiple white spots may indicate a zinc issue, but they need to be on lots of nails and plentiful, plus trauma can also give white spots.
Also poor healing can be a sign of zinc issues and poor skin health like acne and atopic dermatitis


ACTIONS TO TAKE:
– Always get the patient to get GP’s blood tests and look for ALP levels under 70iu/L.
– Consider the level in reflection of their symptoms, 30 mg of zinc citrate or picolinate will be a good trial treatment
– Always keep zinc acetate lozenges from Life Extension in the cupboard.
